Managing a modern medical practice requires balancing exceptional patient care with the grueling demands of administrative and financial operations. For many healthcare providers, the complexities of the revenue cycle — ranging from medical coding to denial management — become a significant drain on internal resources.
This is why outsourcing medical billing has emerged as a transformative strategy for clinics aiming to maintain financial health while reducing the burden on in-house billing staff. By partnering with third-party professionals, practices can streamline their claims process and ensure timely insurance reimbursements.
Highlights
- Compliance Security: Professional billing services stay updated on ever-changing HIPAA regulations and payer requirements to minimize audit risks.
- Financial Growth: Outsourcing frequently leads to improved cash flow and a significant reduction in billing errors that lead to claim rejections.
- Cost Efficiency: You can eliminate the overhead of high salaries, benefits, and expensive billing software by using a scalable, flat-rate model.
- Expert Oversight: Access to specialized coding specialists ensures that CPT codes and ICD-10 requirements are met with precision every time.
- Operational Focus: Transitioning to external experts allows your clinical team to prioritize patient encounters rather than paperwork.
What Is Medical Billing?
Medical billing is the essential process of submitting and following up on insurance claims to receive payment for services provided by healthcare professionals. It acts as the bridge between a patient encounter and the practice’s financial reimbursement.
Efficiently managing this cycle ensures that a medical practice remains financially viable while continuing to serve its community.
Key Components of the Medical Billing Cycle
The medical billing process is a complex cycle that requires precise coordination between administrative staff, clinicians, and insurance entities. When any part of this chain breaks, the resulting payment delays can significantly impact the clinic’s financial health.
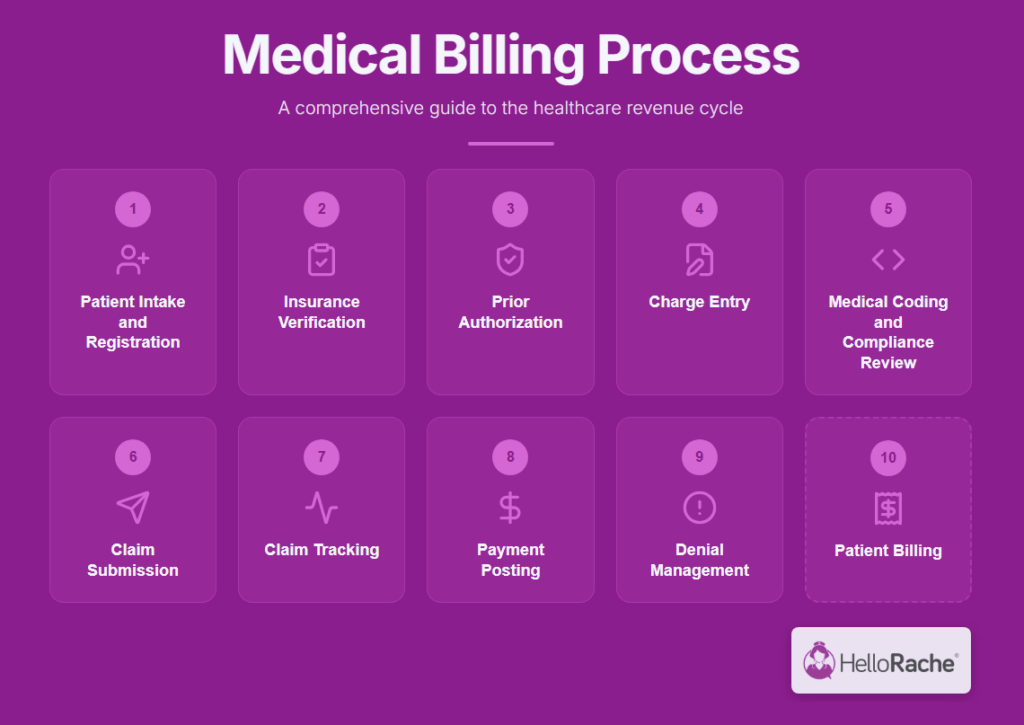
The process involves:
- Patient Intake and Registration: Capturing accurate patient demographics and insurance information at the first point of contact.
- Insurance Verification: Confirming eligibility and benefit levels before the patient’s visit to ensure coverage.
- Prior Authorization: Obtaining advance approval from the health plan using the verified insurance data to ensure the service qualifies for payment.
- Charge Entry: Assigning a monetary value to the performed services based on the established practice fee schedule.
- Medical Coding and Compliance Review: Translating clinical notes into standardized CPT, ICD-10, and HCPCS codes by coding specialists while performing a coding review to ensure billing compliance.
- Claim Submission: Sending the coded claim to the insurance companies through a secure clearinghouse or billing system.
- Claim Tracking: Monitoring the status of every submitted claim through every stage of the adjudication process to identify bottlenecks or payment delays before they negatively impact the practice’s cash flow.
- Payment Posting: Entering the received insurance reimbursements and patient payments into the practice management software.
- Denial Management: Identifying denied claims, investigating the cause, and resubmitting appeals with corrected information.
- Patient Billing: Generating and sending patient bills for any remaining balances, such as deductibles or copayments.
Focusing on these specific administrative tasks allows the billing team to maximize revenue while minimizing errors. When these steps are handled with expertise, the practice can maintain a much healthier revenue cycle.
Challenges Facing In-House Medical Billing
Managing this intricate cycle internally places an immense burden on a medical practice. From staffing challenges to the rising complexity of payer requirements, in-house teams often struggle to maintain industry standards for efficiency.
- Submission Complexity Increases as Data Quality Declines: Nearly seven out of ten (68%) healthcare providers report that submitting “clean” claims is significantly more challenging today than it was just one year ago. At the same time, more than one in four (26%) revenue cycle leaders report that at least 10% of their denials are due to inaccurate or incomplete data collected during patient intake. (source: Experian).
![Graphic showing The Denial Accelerator: [Bad] Data Quality](https://hellorache.com/wp-content/uploads/2026/01/image-12-1024x576.png)
(Source of data: Experian)
- Productivity and Documentation Gaps: In 2024, surgical specialists in private practice saw a 15.44% decrease in median work Relative Value Units (wRVUs) despite a massive 105% increase in total encounters, signaling significant issues with undercoding or documentation gaps (source: MGMA).
- Increasing Payer Scrutiny: Denials stemming from questions of medical necessity increased by 5.0% in 2024, while requests for more information (RFI) rose by 5.4% (source: Becker’s Payer Issues). This reflects a much tighter environment for insurance reimbursements.
- Staffing and Administrative Burden: On average, practices now complete 39 prior authorizations per physician, per week, a task that consumes approximately 13 hours of staff time weekly and leads to physician burnout in 89% of cases (source: AMA).
These obstacles create a high-pressure environment for billing staff, often leading to:
- Poorer healthcare outcomes
- Reduced patient care
- Physician burnout
When internal resources are stretched thin, the medical office risks losing substantial revenue to avoidable claim rejections and payment delays. Outsourcing medical billing offers a way to solve most of those issues.
Benefits of Outsourcing Medical Billing
Choosing to move your billing operations to a specialized third-party company can provide a massive boost to your bottom line. It transforms a high fixed cost into a lower variable one that scales with your patient volume.
Here are the main benefits of outsourcing medical billing.
Financial and Operational Benefits
Transitioning to external billing and revenue cycle management can immediately free up capital that was previously tied up in administrative overhead. These benefits extend from the back office to the bank account:
- Improved Cash Flow: External teams focus solely on timely filing, ensuring that money flows into the medical practice without the typical payment delays of an overworked office.
- Enhanced Efficiency: Professional services use automated billing and cloud computing services to process claims significantly faster than traditional manual methods.
- Scalability: As your practice grows, your billing partner can handle the increased volume of insurance submissions without you needing to hire new employees.
- Cost-Effectiveness: You save on the cost structure of office space, hardware, and the annual software licensing fees required for a robust billing platform.
- Increased Revenue: Experts capture more revenue by identifying under-coded visits and aggressively pursuing every dollar from insurance reimbursements.
Expertise and Compliance Benefits
Staying current with ever-changing payment policies and federal regulations is a full-time job in itself. Outsourcing brings:
- Access to Expert Knowledge: You gain a team of third-party professionals who stay informed on the latest Healthcare Financial Management Association guidelines.
- Better Compliance: Dedicated partners adhere to strict compliance protocols and healthcare laws, protecting you from potential fraud and abuse risks.
- Reduced Errors: Specialized coding review processes minimize the billing errors that often lead to costly claim denials or rejections.
Practice and Patient Benefits
When you lift the burden of paperwork, the quality of care often sees a measurable improvement:
- Advanced Technology: Outsourcing gives you access to high-end billing software and AI-powered systems that might be too expensive for a private practice to buy.
- Patient Satisfaction: When billing is handled accurately and professionally, patient dissatisfaction regarding confusing bills or insurance errors decreases.
- Data and Reporting: Professional services provide comprehensive accounts receivable management reports, giving you a clear view of your financial health.
- Focus on Patient Care: When doctors and office managers stop worrying about revenue cycles, they can reinvest that energy into the patient experience.
Potential Downsides of Outsourcing
While the benefits are extensive, any strategic shift in financial operations requires a careful look at the risks involved.
Loss of Control Over Operations
Relinquishing daily oversight of your billing tasks can feel like a major change for hands-on office managers:
- Incompatible Systems: If the billing company uses different billing platforms from your existing electronic health records, data transfer can become a bottleneck.
- Vendor Prioritization: A large medical billing management firm may prioritize its largest clients, leaving smaller health centers waiting for support.
- Loss of Control: Some providers feel uneasy when they cannot physically walk down the hall to check on a claim’s status with their billing staff.
Open communication and transparent reporting can effectively mitigate these concerns.
Data and Security
Protecting patient information is a legal and ethical imperative. Security must be the primary focus of any outsourcing agreement:
- Security Lapses: If the vendor does not use high-level encryption or secure cloud computing services, your practice could be liable for a data breach.
- Security Concerns: Sharing sensitive patient data with an external entity always introduces new variables into your security protocols.
- Privacy Risks: Ensuring the partner follows all HIPAA regulations is a non-negotiable requirement to avoid heavy fines and legal trouble.
Impacts on Patient Experience
The way a billing company interacts with your patients can either strengthen or damage your reputation:
- Communication Challenges: If the billing company handles patient queries, a lack of empathy or poor customer service can reflect poorly on your medical office.
- Patient Dissatisfaction: Errors made by the outsourced team can lead to frustrated patients calling your office to complain about their patient payments.
Financial and Performance Issues
Outsourcing introduces a different financial dynamic that your practice must be prepared to manage:
- Dependence on Providers: Your practice becomes reliant on a third-party provider for survival, making the choice of partner incredibly high-stakes.
- Fluctuating Costs: Most companies charge a percentage of collections, meaning your costs rise as your revenue increases, which can affect long-term budgeting.
- Hidden Fees: Some contracts include extra charges for things like denial management, postage for patient bills, or EHR integration setup.
Compliance and Legal Challenges
The legal responsibility for billing accuracy ultimately rests with the provider, regardless of who does the work:
- Compliance Violations: Any failure by the vendor to comply with the National Association of Community Health Centers or federal guidelines can result in devastating audits.
- Fraud and Abuse Risk: If a billing company engages in unethical coding practices to inflate revenue, the healthcare providers are often held legally responsible.
Key Considerations When Choosing a Medical Billing Service
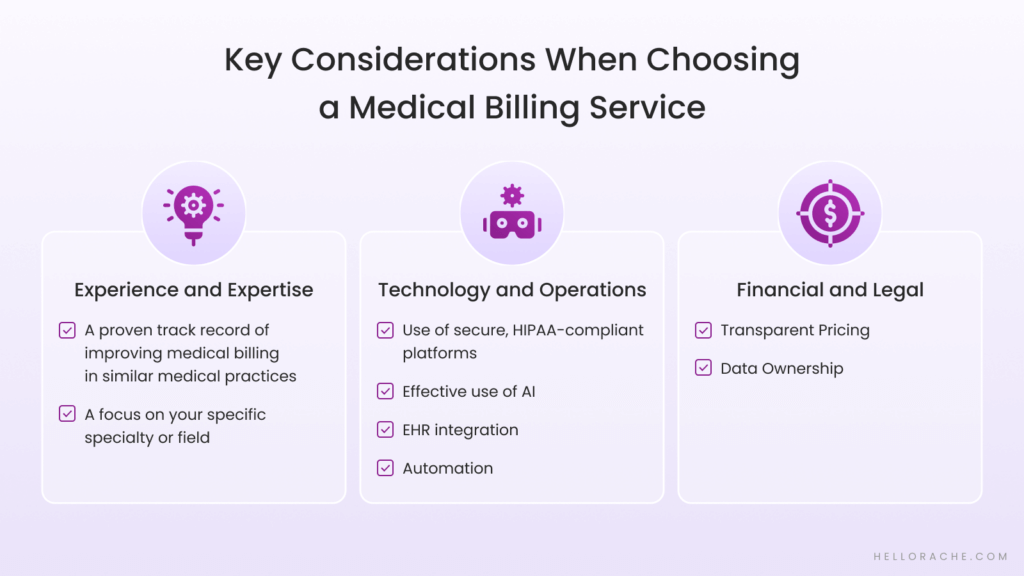
Selecting the right medical billing partner is the most important step in the entire process. You need a team that acts as an extension of your own staff, sharing your commitment to accuracy and professionalism.
Here’s what to look for when vetting virtual assistant partners.
Experience and Expertise
Deep knowledge of your specific clinical niche is non-negotiable for a billing partner. Generalists often miss the subtle nuances that lead to maximum reimbursement. Look for:
- A proven track record of improving medical billing in similar medical practices
- A focus on your specific specialty or field
Experience often dictates how well a company can navigate the complexities of modern payment policies across dental healthcare, optometry, veterinary medicine, and other specialized fields.
Technology and Operations
Look at the tools your billing partner uses. They should make your life easier, not more complicated. Seamless integration is the goal of every modern technical setup. Look for:
- Use of secure, HIPAA-compliant platforms
- Effective use of AI
- EHR integration
- Automation
Reliable technology ensures that your data remains synchronized across all your Practice Management tools. You should also review their business processes and operations for reporting and denial management.
Financial and Legal
Reading the fine print is critical when assessing an outsourced medical billing provider. A few things to look for include:
- Transparent Pricing: Look for a provider like Hello Rache that offers a simple, flat-rate cost structure rather than complex percentage-based fees.
- Data Ownership: You should always maintain full ownership of your patient data and be able to export it if the partnership ends.
Questions To Ask Before Hiring
Before signing any agreement, you should conduct a thorough interview to ensure the service meets your practice’s standards. Use these questions to vet potential candidates effectively.
How Long Have You Been in Business, and How Many Practices Like Mine Do You Serve?
Experience in your niche is vital because billing for a general practitioner differs significantly from billing for a specialized surgeon. A company that serves hundreds of similar medical groups will already be familiar with the common insurance entities in your region.
What Are Your Specific Denial Management and Appeal Processes?
The true value of a billing service lies in how it handles difficult, unpaid insurance claims. They should have a systematic process for reviewing coding errors and resubmitting claims within the timely filing limits set by payers.
Can You Provide References From Similar Practices?
Speaking with other healthcare providers gives you an honest assessment of the vendor’s reliability and customer service quality. Ask these references about the transparency of the reporting and if they have seen a noticeable improvement in their revenue cycles.
What Technology Do You Use, and How Does It Integrate With My EHR?
Seamless integration is necessary to ensure patient data flows from the clinic to the billing system without human error. You want to avoid any “middle-man” software that requires your staff to upload files manually every single day.
What’s Included in the Fee, and Are There Any Hidden Costs?
Ask whether the price covers the cost of sending patient bills or if you will be charged extra for each envelope and stamp. Understand if there are setup fees or long-term contracts that might trap your practice in an unproductive relationship.
How the Outsourcing Process Works
The transition to outsourcing medical billing doesn’t have to be a disruptive event for your medical office. A structured onboarding process helps ensure your revenue cycle management remains stable during the transition.
Step 1. Assessment and Audit of Existing Accounts
The first step is a deep dive into your current financial health. A quality partner will review your aged accounts receivable to identify current bottlenecks.
Step 2. Technical Integration With EHR and Billing Systems
Next, the technical teams will work together to establish secure, real-time links between your office and the billers. This ensures that, as soon as a doctor finishes a note, the biller can see it and begin coding.
Step 3. Staff Training and Workflow Alignment
Even with an external partner, your in-house team needs to know how the new system works. This phase involves setting clear expectations for how you’ll share data and who is responsible for specific patient queries.
Step 4. Go-Live and Continuous Monitoring
Once you flip the switch, the focus shifts to monitoring the success of the new claims-handling process. You should expect to see a higher percentage of “clean claims” right from the start.
Managing the Relationship
Maintaining a healthy partnership requires regular check-ins and shared data. Treat your billing partner as an extension of your own staff by providing consistent feedback. Regular meetings to review industry reports can keep both teams informed about broader industry shifts.
How Outsourcing Works With Hello Rache
Hello Rache offers a unique and highly efficient approach to outsourcing medical billing. We don’t operate like a traditional, faceless billing factory that treats your practice like a number. Instead, we provide a dedicated Medical Billing Virtual Assistant who works as an integrated member of your team.
Our assistants are registered nurses or medical professionals who understand the nuances of CPT codes and healthcare laws. Because they work in your software in real-time, there’s no delay in payment posting or insurance submissions. You get the expertise of a professional biller with the loyalty of an in-house employee.
We keep our pricing simple:
- You pay a flat rate of $9.50 per hour for your Healthcare Virtual Assistant®
- No setup fees and no long-term contracts
This allows you to scale your administrative support up or down based on your current practice goals, with no financial risk.
Future Trends in Medical Billing Outsourcing
The healthcare finance landscape is shifting rapidly toward digital integration. Several key trends will define how successful practices manage their revenue in the coming years.
Technological Advancements Influencing the Industry
The tools we use to manage revenue are becoming smarter and more intuitive. These advancements are helping to eliminate many of the manual errors that used to plague the industry, and include:
- Cloud computing services that will continue to make remote billing support more reliable
- Blockchain technology to handle patient data and verify insurance claims
- AI-powered systems that predict claim denials before they even happen
The Growing Importance of Data Analytics
In the modern medical office, data is more than just numbers. It’s a roadmap for future success:
- Detailed reporting on patient demographics and payer requirements will continue to improve the billing process
- Practices will move beyond simple spreadsheets to advanced healthcare revenue management dashboards
- Predictive analytics will help office managers forecast cash flow with incredible accuracy
Emerging Global Markets for Medical Billing Outsourcing
The search for talent has gone global. It provides American practices with access to highly skilled professionals at a fraction of the local cost. Global partners like Hello Rache offer:
- Highly educated medical professionals in regions like the Philippines
- Significant cost savings while maintaining industry standards
- A way to maintain 24/7 operations
By looking globally, your practice can find the specialized talent it needs without the high overhead of a domestic hire.
Conclusion
Outsourcing medical billing is no longer just an option for large hospitals. It’s a strategic necessity for any medical practice that wants to thrive in a competitive environment. While there are considerations regarding control and data security, the financial and operational benefits far outweigh the potential downsides.
By selecting a partner that offers transparent pricing, specialized expertise, and seamless integration, you can protect your practice’s financial health. This move allows you to refocus on what truly matters: providing world-class care to your patients.
If you’re ready to eliminate billing stress and maximize your revenue, we’re here to help you make the transition.
FAQs About Outsourcing Medical Billing
Will I Lose Control Over My Practice’s Finances?
No, you actually gain more visibility into your finances through regular, detailed reporting. A professional partner acts as your eyes and ears, alerting you to trends that you might have missed in-house.
You retain full ownership of your data and can monitor the billing process in real time through your EHR integrations.
Is Outsourcing Medical Billing HIPAA-Compliant?
Yes, reputable companies like Hello Rache prioritize compliance regulations and use secure, encrypted platforms. Our Healthcare Virtual Assistants® undergo rigorous HIPAA training to ensure all patient data is handled with the highest level of security.
How Long Does It Take To See Results From Outsourcing?
Most practices see an improvement in their timely filing and claim submission rates within the first 30 days. As the backlog of denied claims is cleared, you’ll notice a steady increase in your insurance reimbursements.
That said, the reduction in administrative stress for your clinical staff is often felt almost immediately after the onboarding is complete.