Medical documentation refers to creating, storing, and retrieving medical records. It is a vital part of the healthcare industry, as it helps to ensure that patients receive the best possible care.
Medical documentation can be used to track the progress of a patient's treatment, monitor the effectiveness of treatments and medications, and provide information for research purposes. However, doing all this can be tedious.
Healthcare providers need to hire administrative staff to manage their medical documentation. The administration staff ensures that medical records are accurate and up to date. In this guide, you'll learn more about medical documentation and who you can entrust with this responsibility.
What is medical documentation?
Medical documentation includes evidence and information about a patient's medical history, diagnoses, treatments, and outcomes used to make decisions about their care.
The documentation can be in paper records, electronic health records (EHRs), or a combination of both.
Medical documentation must be accurate, up-to-date, and complete so that healthcare professionals can use it to make the best patient care decisions.
Conversely, inaccurate, outdated, or incomplete medical documentation can lead to a diagnosis, treatment, and billing errors.
Clinicians, such as doctors, nurses, and therapists, create medical documentation. However, patients and their families also play an essential role in creating and maintaining accurate medical records.
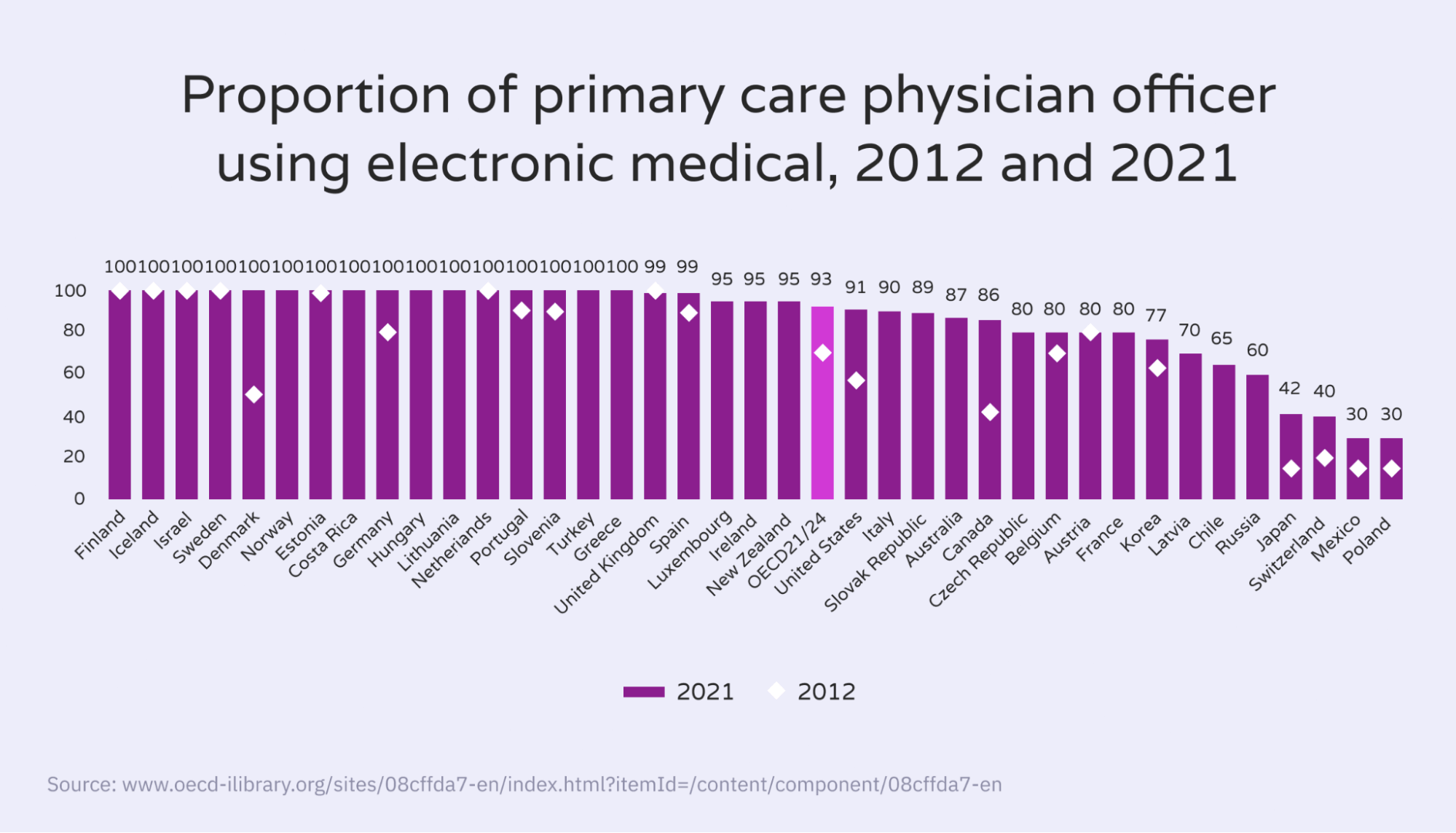
OECD (Organization for Economic Co-operation and Development) data shows that the number of primary care physicians using electronic medical records has increased in the past decade.
Did you know Hello Rache's qualified virtual assistants can save your business more than 50% while providing an improved quality of care and ensuring all your calls are answered promptly and efficiently? Learn how it works here.
Importance of medical documentation
Clinical documentation is vital for several reasons. First, it provides a record of the care provided to a patient. It is crucial not only for continuity of care but also if a patient needs to be seen by another provider or there is a question about the care provided.
Second, it is used for billing purposes. For a provider to be reimbursed by insurance, documentation must show what services were provided and that they were medically necessary.
Moreover, providers can use documentation to track care outcomes and identify improvement areas.
Finally, documentation is essential if a provider is ever accused of malpractice. In a lawsuit, documentation can show what was done (or not done) and why.
What constitutes a medical document?
A medical document is any document that contains information related to a person's health or medical history. For example, it can include a simple doctor's note to a complex hospital discharge summary.
Medical documents are a vital part of a person's medical record and can be used to help make decisions about diagnosis, treatment, and care. Here are some standard medical documents:
- PIL (patient information leaflet): A PIL contains information about a medication, such as how to take it and what side effects it may cause.
- Medical history record: The patient's medical history includes information about past illnesses, surgeries, and vaccinations.
- Discharge summary: It's a clinical document prepared by a doctor when a patient is discharged from a hospital stay. It includes information about the reason for the hospitalization, procedures performed, and the patient's diagnosis and prognosis.
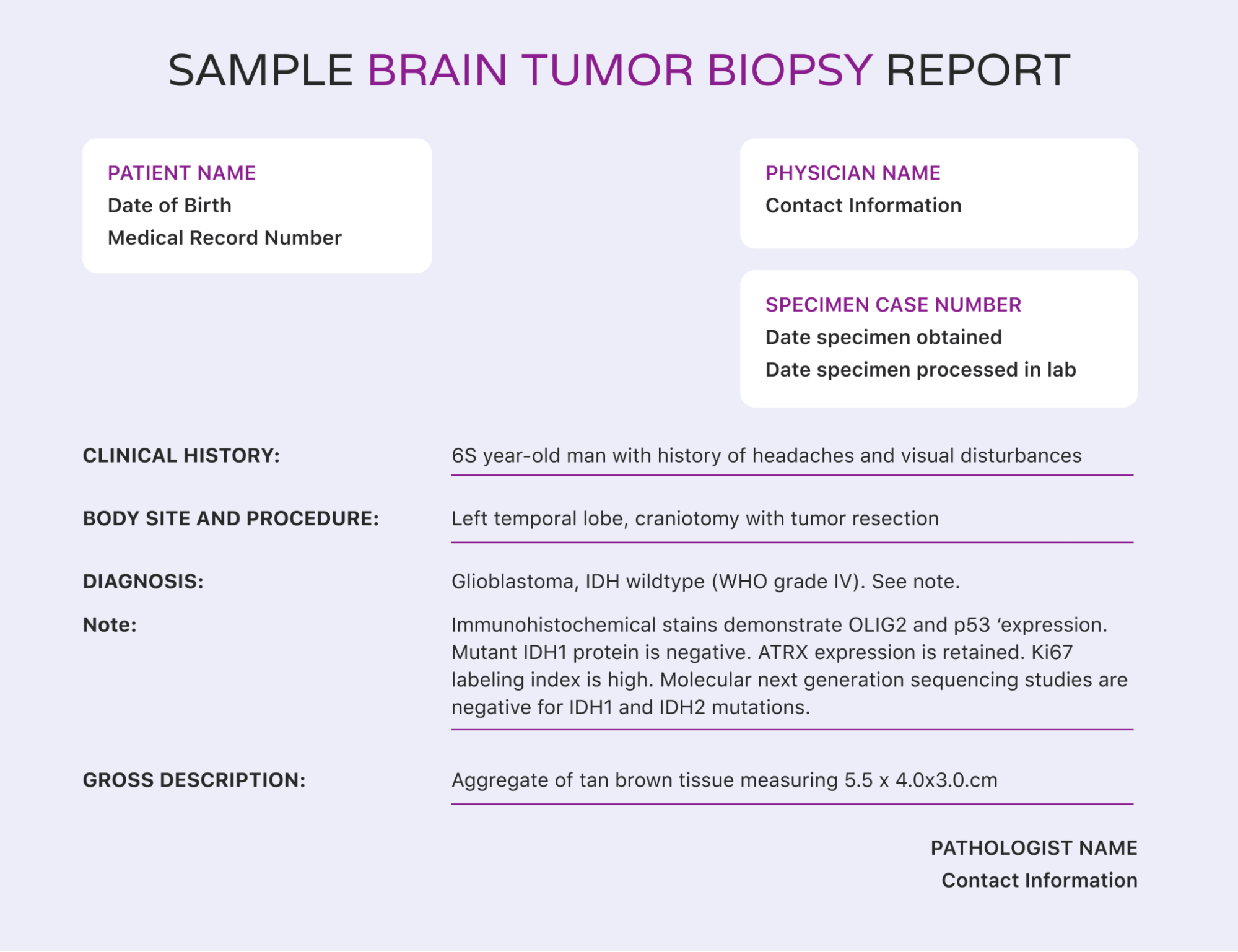
- Lab results: Lab results are records of tests performed on samples of blood, urine, or other tissues.
- Imaging reports: An imaging report is a document that describes the findings of an X-ray, MRI, or other imaging tests.
- Referral Letter: A doctor may write a referral letter to another doctor or specialist to request an appointment for a patient.
- Progress notes: Progress notes are written updates from doctors, nurses, or other healthcare team members. They document a patient's condition and response to treatment.
- Insurance forms: Patient insurance forms may be required to reimburse medical expenses.
While these are the standard documents, other clinical forms may also be categorized as medical documentation.
Who manages medical documentation?
CDC (Centers for Disease Control) data shows that 89.9% of office-based physicians were using an EMR/EHR system in 2019. However, there are still a few hurdles in implementing electronic health records. That’s why healthcare facilities need specific staff for managing documentation.
In a healthcare setting, medical documentation is typically managed by medical transcriptionists, medical records technicians, or health information technicians.
For instance, medical transcriptionists may have to listen to doctors' audio recordings and convert them into written reports. These reports become part of a patient's medical records.
Likewise, medical records technicians may have to organize and categorize different types of medical records. They might also be responsible for managing the release of these records to authorized individuals.
These professionals ensure that patient medical records are accurate and up-to-date. They may also have to code patient medical records for insurance purposes.
Why is good medical documentation necessary?
Medical records are much more than merely a doctor's scribbled notes (in barely legible handwriting). Instead, they are a crucial part of a patient's medical history and play an essential role in informing doctors about the best course of treatment.
Good medical documentation can help ensure that patients receive the best possible care. Here are some reasons proper medical documentation is necessary for a healthcare setting.
- Acts as proof of services provided: Healthcare professionals can use medical documentation to show what services were rendered to a patient. This information can be important for billing and insurance purposes.
- Is a legal document: Medical documents hold up as legal evidence in court if a patient sues a healthcare provider.
- Can be used for research: Data from medical documentation can be used to improve treatment methods or develop new ones. For instance, researchers can elucidate the patients' response to a particular medicine by analyzing their progress reports.
- Aids in the continuity of care: Medical documents, such as imaging reports, can help specialists provide a second opinion about a patient's condition. The information can also be shared with other healthcare providers to provide continuity of care.
- Is a means of reimbursement: Insurance companies often use medical documentation to determine if they will reimburse a patient for treatment.
Elements of excellent medical documentation
Adequately recorded and up-to-date medical documents have a few significant components. Here are some of them:
- Date and time: The doctor, nurse, or other medical professionals should document the date and time of every entry. Doing this is critical in case of discrepancies or questions about the care given.
- Role of the document creator: The document creator should specify their part in the healthcare facility. It could be anything from "family physician" to "registered nurse."
- Patient information: The medical document should have the patient's name, age, gender, and other relevant demographics. If the patient is a minor, the document should also include the name and contact information of the child's parent or guardian.
- Assessment of the patient's condition: Whoever creates the document should include an honest review of the patient's condition. They must include any changes in the patient's condition since the last time they were seen. For example, if the doctor changes the treatment plan, they should mention it clearly.
- Legibility: The document's legibility is essential in case another healthcare professional needs to review the document or if it ends up in court.
- Professional tone: Medical documents must be written or recorded in a professional manner. Slang, abbreviations, or acronyms that could be misunderstood should be avoided.
- Usage of approved abbreviations: Healthcare professionals should only use widely accepted abbreviations in their documentation so that other professionals can understand them.

- Signature and credentials: The document should be signed and dated by the healthcare professional who created it. They should also include their credentials (degree, license number, etc.) so that their identity can be verified.
While these are some general rules, every hospital or healthcare facility may have its own protocol for writing medical documents.
How to document different interactions in a healthcare setting
Besides consults, there are many types of interactions between providers and patients. The interaction will determine what the doctor will document in the patient’s record.
Phone conversation
General practitioners (GPs) and other healthcare providers frequently have phone conversations with patients. These conversations may be about:
- Results of tests or investigations
- Changes to medication
- Appointment times and locations
- General inquiries
Family meetings
A family meeting is a discussion between a healthcare provider and the patient’s family about the patient’s condition, treatment, and prognosis. Family meetings may be held:
- When a patient is admitted to the hospital
- When a patient’s condition changes
- At the request of the patient or their family
- During discharge planning
Discharge summary
The discharge summary includes:
- The patient’s name, address, and next of kin
- The dates of admission and discharge
- An overview of the patient’s condition, treatment, and progress while in hospital
- Information about any follow-up appointments or tests
- Medication changes
- Relevant test results
Mistakes
Healthcare providers also need to document when they make a mistake. It could be:
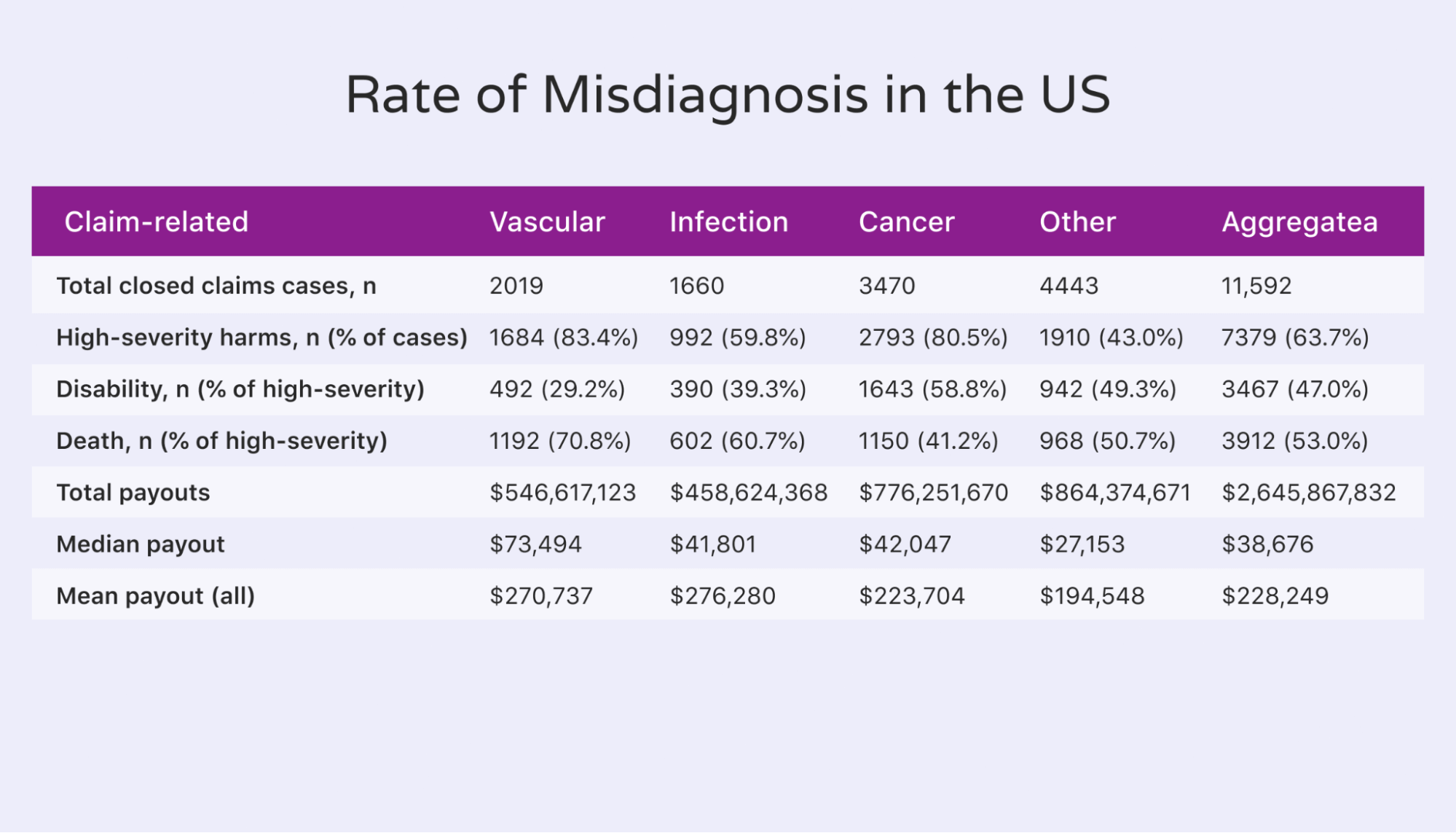
- A wrong diagnosis (1 in 3 misdiagnoses lead to serious injury or death)
- An incorrect test or investigation
These documents prove helpful if the patient decides to file a medical malpractice claim in the future.
How to use the SOAP method for medical documentation
SOAP (Subjective, Objective, Assessment, and Plan) is a mnemonic acronym used by healthcare providers to document a patient's medical chart. Here's how to implement it:
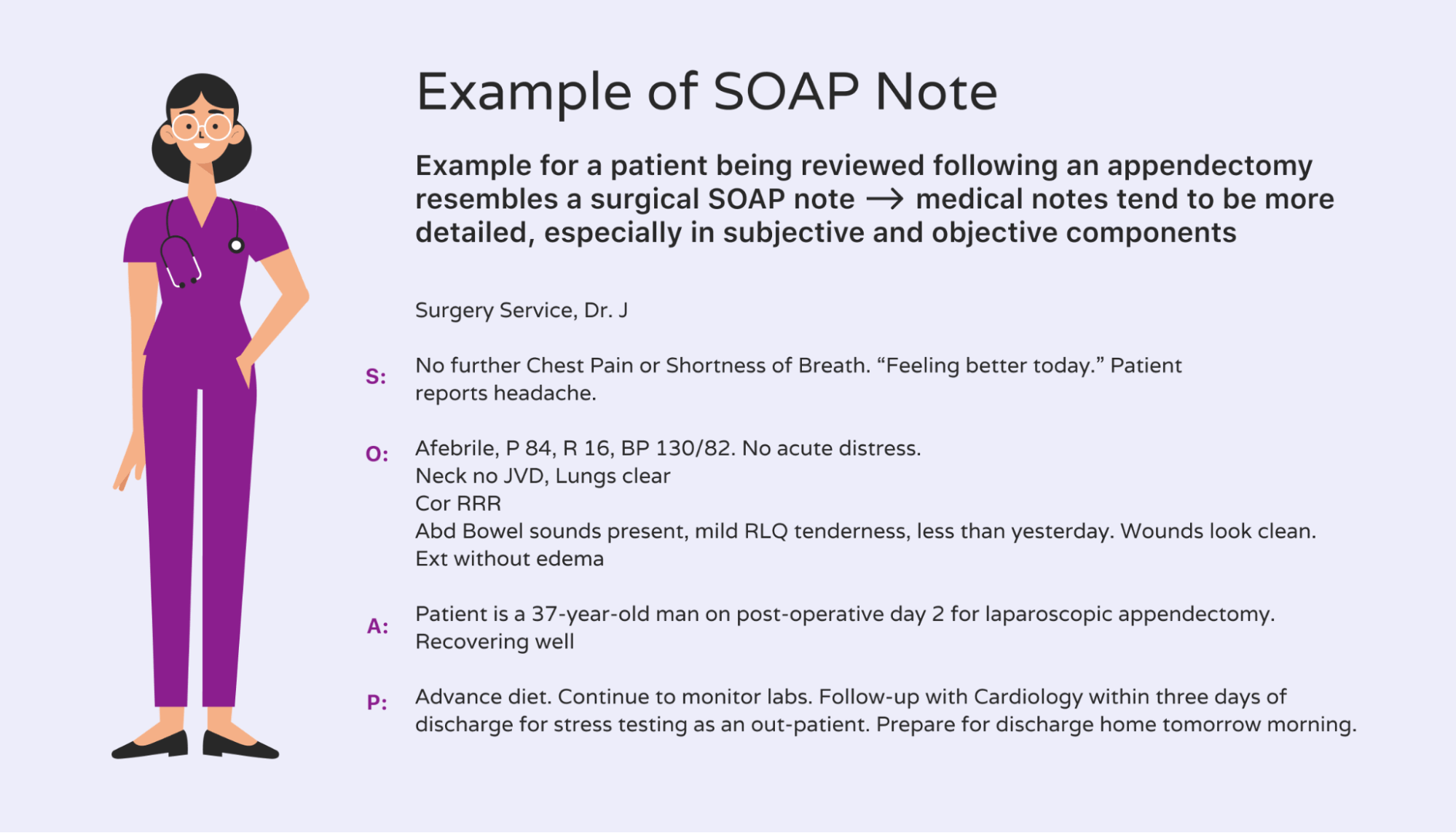
Subjective
The subjective section includes everything the patient has told the doctor about their condition, such as complaints, symptoms, or history of the illness.
When recording the subjective data, it is vital to use the patient's words. Include as much detail as possible.
Objective
The objective section is a factual account of what the healthcare provider has observed during the examination. It may be in the form of physical examination findings, laboratory test results, or imaging studies.
Assessment
The assessment is based on the information gathered in the subjective and objective sections. It is a working diagnosis of what may be wrong with the patient.
For example, if a patient complains of abdominal pain, the doctor will document this in the subjective section.
They will then document objective findings such as decreased appetite, bloating, or nausea. Based on these findings, the doctor may conclude the patient has gastritis.
Plan
In the plan section, the physician will outline the treatment options for the patient, such as medication, referrals to specialists, or lifestyle changes.
It could be as simple as ordering a lab test or prescribing medication. The healthcare professional should also document when and how they will follow up with the patient.
When used correctly, the SOAP method can help ensure all relevant information is captured in the medical record. It can also improve communication between healthcare providers.
How to hire administrative staff to document medical information
When hiring administrative staff for documenting medical information, you will want to consider individuals with previous experience in the medical field.
They don't necessarily have to be medical doctors or nurses, but they should have some understanding of the terminology and procedures used in a medical setting.
Medical transcriptionists and certified coding specialists are often good candidates for this position. You may also want to consider individuals with strong administrative skills who can learn new software programs quickly.
For example, if you use EMR(electronic medical records) in your office, you must look for someone comfortable using new technology. Apart from these basic skills, here are some other things to look for when hiring administrative staff for a medical practice:
- Attention to detail
- Medical knowledge
- The ability to type quickly
- Familiarity with medical coding
- Strong administrative skills
Since the administrative staff will have to work with medical documentation, it will be helpful if they understand medical terminology and are familiar with standard abbreviations.
Hire a virtual assistant for medical documentation
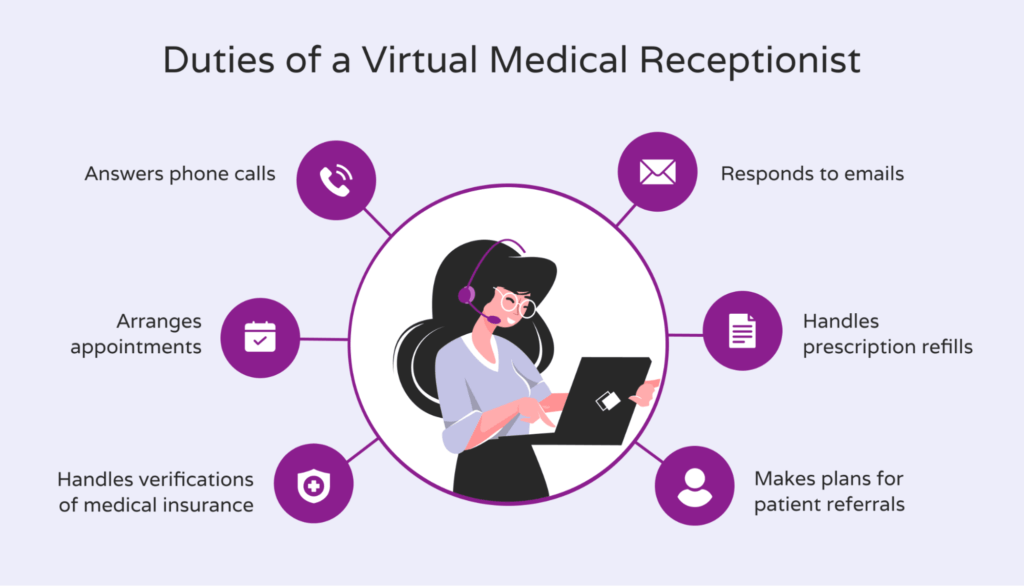
A virtual healthcare assistant can manage several tasks in a healthcare facility, such as scheduling appointments, managing medical records, and providing customer service.
As already established, proper medical documentation is imperative to continuously provide optimal healthcare to patients.
Therefore, medical facilities can hire virtual assistants to organize, manage, and maintain medical records. If you're on the search for the best medical virtual assistants, get a consultation from Hello Rache today. All our VAs have previous experience or education in the medical industry (many are registered nurses), which makes them perfect for medical transcriptionist tasks.
And since all Hello Rache virtual assistants are HIPAA-certified, you can be assured that your patients' privacy will always be safeguarded.